letters to little liberte: 02
/hi adeline,
It’s been more than 4 months since I wrote your first letter — and you’re almost 4 months old. I can’t believe it. At the time I wrote you that letter, I had no idea you would come a week later. We wanted you to stay in for much longer! But I’ll save your birth story for another day.
I’ve felt called recently to document our breastfeeding journey. And apparently, it’s breastfeeding awareness month. Our journey has NOT been easy, but it has definitely been worth it. As I sit here writing this, you’re nursing — and we’re both loving every minute of it. ❤️
You showed strong rooting cues in the NICU, from very early on — like 32 weeks gestational age! All the nurses and doctors kept saying you acted older than your age and would most definitely be a primarily — or exclusively — breastfed baby. you just “got” the boob much easier than the bottle. It came more naturally to you and you had many fewer negative events (cough/choke episodes) on the boob vs. on the bottle. The problem was you were just so little and not yet strong enough to take everything you needed from the boob. So even though we would practice breastfeeding in the NICU, you still got the majority of your feeds from first the feeding tube and then the bottle. Even on the bottle, it took you until almost 38 weeks gestation to conquer eating well enough on your own to be able to go home.
It was always my goal to exclusively breastfeed you. Especially after such a tumultuous and scary pregnancy experience — I just wanted this one “normal” experience. So from the moment you were born, I started pumping around the clock. It was hard work just to get one drop. My milk didn’t come in when they said it should. There was a lot working against us — I had severe health issues and was on a cocktail of meds, you came via emergency c-section and very early at just 30 weeks, and I couldn’t breastfeed you in the NICU for the first 1.5 weeks while you were on the CPAP machine. But I remember the night you came, the neonatologist told us my milk was the best medicine for you. So pump around the clock I did and Tim and I ran daily down to the NICU to bring you those precious little drops. I didn’t even think they could really use them, but they did — the nurses would help us give them to you as oral care on your lips and just inside your mouth. It was wonderful and I was so proud of those drops.
So I kept pumping day in and day out and was constantly playing catch-up with your milk intake (because you were gaining weight like a champ!). And we did as much skin-to-skin as possible every day. There wasn’t one day I didn’t spend with you. I felt lucky that I was able to take leave, that I had access to wonderful lactation support in the NICU, and that I had supportive family and friends giving me tips along the way. Highly recommend getting some “breast” friends for breastfeeding support! I’ll be yours if you’re searching ☺️ It is not easy or natural for everyone!
The first two weeks pumping at home at night I couldn’t even go in your nursery. Staring at your empty crib while pumping was just too much. But eventually, as you kept hitting milestones and getting stronger and healthier, I made it my sanctuary and it brought me peace to be in there knowing we could bring you home soon. I vividly remember sitting in there pumping at night while your daddy was with you, anxiously awaiting a text from him — if it was a picture, I knew it was going to be good news, an empty bottle (one step closer to going home!).
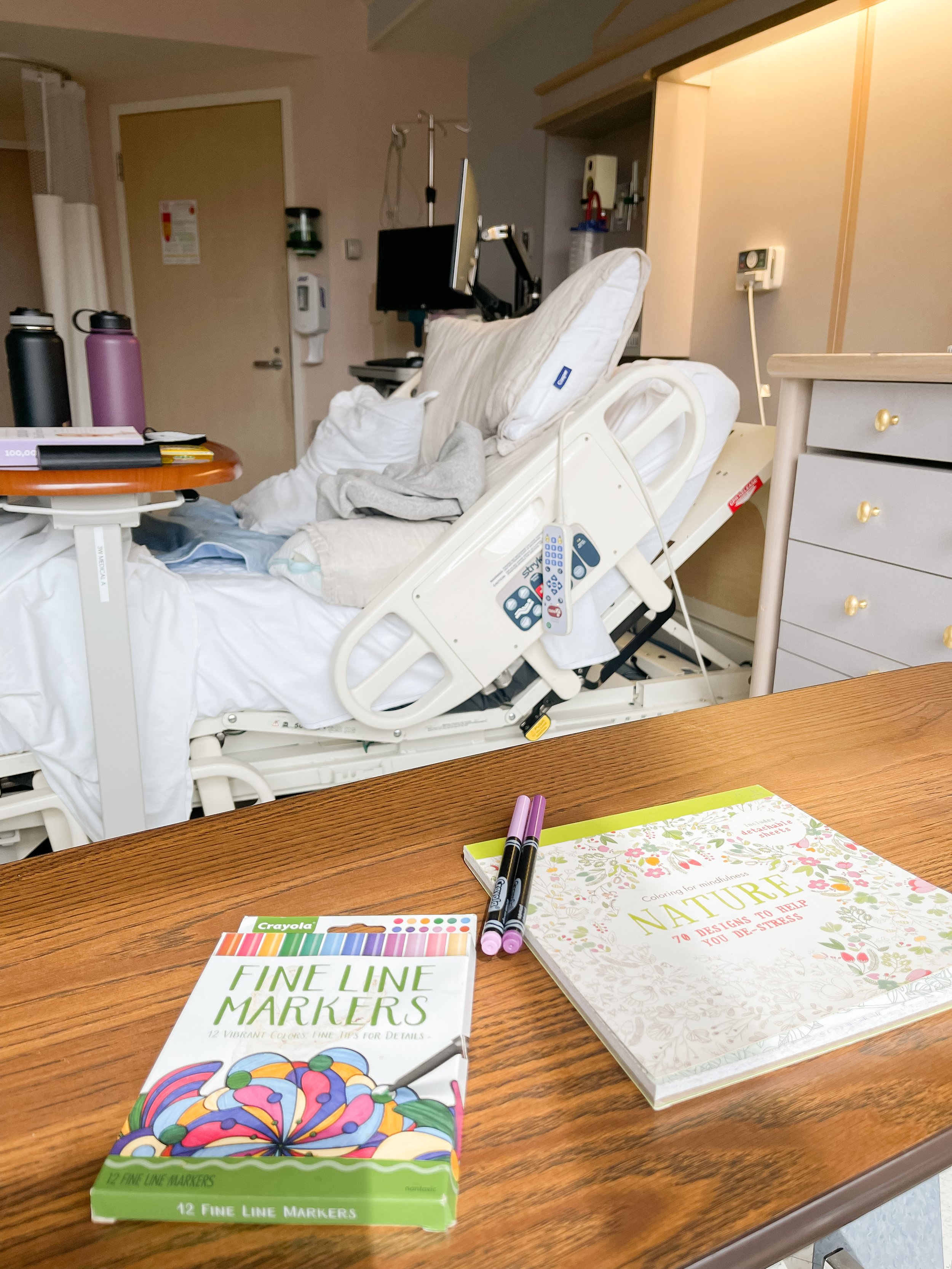
You kept having events on the bottle so one of our favorite doctors recommended we do a 24-hour breastfeeding “test” to see how much you were taking at each feed — maybe you were doing better on the breast than we thought! So we did the test that weekend and the most you took in one feed was 26mL (great for you!!), but it was only roughly half your feed and the majority of feeds you took 8-15mL. So we just kept practicing and focused more on you getting the hang of the bottle.
I hate that we had to choose bottle or breast. And the doctors kept telling us we didn’t have to choose — they wanted to support our breastfeeding journey. But the NICU is a weird place. It’s so metrics-driven and not at all a normal or natural place to establish breastfeeding. There are lots of rules (spoken and unspoken) — and even though we were told you’d be such a good breastfeeder, we were also told that in order to go home, you would have to prove you could take a certain amount via bottle — and whatever additional you took via breast was just a bonus. But that’s not how babies eat. They of course weren’t going to send you home unless you took enough volume in the bottle, but you’re only going to eat until you’re full — so trying to breastfeed you and meet that metric wasn’t going to work. You just weren’t strong enough to do both and we so desperately wanted you to come home.
So to get you home we did just a few minutes on the boob (like 5 minutes or less to keep you motivated and hungry) while I was there and then finished your feed with the bottle. When we finally took you home, we were doing the same thing — boob for a bit and then finish with the bottle. But we kept working with a lactation nurse at the hospital’s Mother Baby Clinic to increase our nursing sessions one at a time. We did weighted feeds while we were there, which gave me the confidence that you are in fact getting what you need! I was convinced I would never get a full milk supply given our uphill battle, and yet here we are — exclusively breastfeeding! It took us until about 3-4 weeks ago, but we did it baby girl.
I’m so incredibly grateful for all the help and encouragement I had along the way. I don’t know why the struggles of breastfeeding aren’t talked about more. It seems like it’s glamorized in film and TV — and of course on social media — and I know our struggles were outsized, but I haven’t spoken to one person honestly who hasn’t said it was a struggle in some way.
Here are some moments I never want to forget:
The way you smile mid-suckle
The way you sigh in satisfaction when I lay you back down to go to sleep
The way you nurse yourself to sleep
The way you just know what to do
The way our bodies just work in harmony
The way the boob is the solution to all problems
Love you forever, my baby girl. Thanks for choosing me as your mama 💞
PS: if you’re reading this and you chose not to breastfeed or it wasn’t a choice and you can’t breastfeed, I see you. You are just as brave and just as wonderful of a mama as any other mama. Don’t let society tell you that you “failed” because the truth is you are doing what’s best for you and your baby and that’s all that matters.
PPS: I describe our experience as “breastfeeding” but recognize that it comes in all forms. Pumping is breastfeeding. Nursing for bonding is breastfeeding. Everyone has their own unique journey!